Choosing a Private Psychiatrist in Cardiff: What Actually Matters
January 17, 2026
What Is Generalised Anxiety Disorder? The Truth About Living With Constant Worry
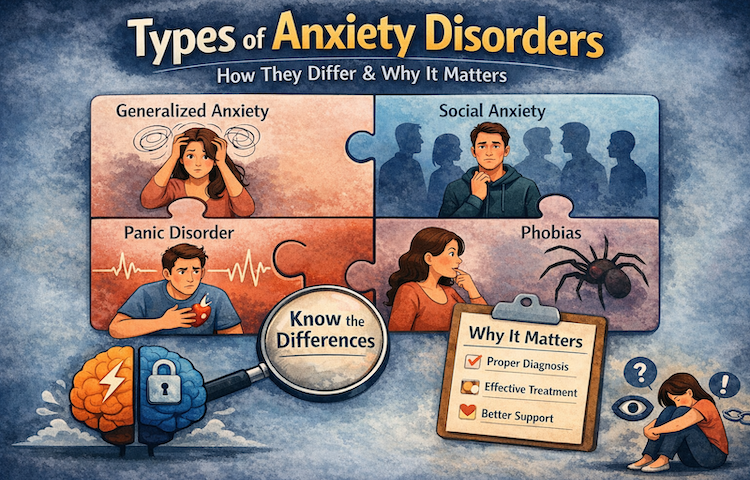
January 22, 2026Treating “anxiety” without knowing which type you have is like treating “pain” without knowing if it’s a broken bone or a stomach ulcer.
Both hurt. Both need treatment. But the approach? Completely different.
Yet here’s what happens in most GP appointments: 15 minutes, a quick chat, maybe a PHQ-9 questionnaire, and you walk out with a prescription for sertraline and a leaflet about breathing exercises.
No discussion about whether your anxiety hits you in sudden waves of terror or sits like a constant weight in your chest. No exploration of whether you’re avoiding the Tube because of panic attacks or because you’re terrified of being judged by strangers.
Just “anxiety.”
Let’s fix that. This article breaks down the seven clinically recognised anxiety disorders, not because you need a diagnosis to validate your suffering, but because understanding which type you’re dealing with changes everything about what actually works.
What Anxiety Disorders Are (And Why “Just Anxiety” Isn’t Enough)
The difference between normal anxiety and a disorder
Look, anxiety itself isn’t the problem.
Anxiety before a job interview? Normal. Nerves before a first date? Expected. That flutter in your stomach before presenting to your team? Your brain doing exactly what it evolved to do.
Here’s where it crosses the line into a disorder:
The anxiety is excessive, wildly out of proportion to the actual threat. You’re not nervous about the presentation; you’re convinced you’ll have a heart attack during it.
It’s persistent, it doesn’t switch off when the stressor passes. The interview ended three days ago, but your mind is still replaying every awkward pause.
It’s impairing, you’ve started calling in sick to avoid meetings. You’ve turned down promotions. You’re making life decisions based on what keeps the anxiety at bay.
Anxiety disorders aren’t defined by having anxiety. They’re defined by anxiety that’s hijacked your life.
Why lumping all anxiety together causes real damage
Here’s the truth about treating anxiety as one monolithic thing:
Different anxiety disorders are driven by different mechanisms in the brain. Generalized Anxiety Disorder involves chronic worry circuits that won’t shut down. Panic Disorder is about fear of your own physical sensations. Social Anxiety Disorder is rooted in perceived judgment and rejection.
Same word. Completely different problems.
When your GP prescribes the same SSRI for all three, they’re not being negligent, they’re working within a system that doesn’t have time for nuance. But you end up feeling like treatment “didn’t work” when really, the treatment wasn’t matched to your specific condition.
Here’s what proper identification changes:
- Medication responses differ between disorders
- Therapy approaches must be targeted (exposure therapy for phobias looks nothing like CBT for GAD)
- Prognosis depends on early, accurate intervention
- You finally feel understood instead of dismissed
Let’s separate the seven types of anxiety disorders.
Generalised Anxiety Disorder (GAD): When Your Brain Won’t Stop Planning for Disasters
What GAD actually looks like
Imagine your mind as a browser with 47 tabs open, each one playing a different disaster scenario.
That’s GAD.
Generalised Anxiety Disorder is characterised by excessive, pervasive worry across multiple areas of life. The worry shifts constantly, from your health to your finances to your relationships to whether you locked the door this morning.
Common features include:
- Relentless “what if” thinking that exhausts you
- Overestimating risks and underestimating your ability to cope
- Chronic muscle tension (hello, permanent tight shoulders)
- Sleep disturbance, either can’t fall asleep or wake at 3am with your mind racing
- Mental fatigue and irritability from the constant background noise
Here’s the crucial difference: GAD isn’t tied to specific situations. You’re not anxious about flying or public speaking. You’re anxious about everything, all the time.
How GAD differs from normal worrying
Everyone worries. That’s not GAD.
Here’s the difference:
Normal worry is temporary. You’re stressed about an exam, you take the exam, the stress resolves. In GAD, you pass the exam and immediately start worrying about the next one. Then about whether you actually passed. Then about what happens if you didn’t pass.
The worry is free-floating, it attaches itself to whatever’s available. Solve one problem, your brain finds another.
Reassurance provides only brief relief. Someone tells you “it’ll be fine,” you feel better for 20 minutes, then the doubt creeps back.
GAD often develops gradually. You don’t wake up one day with it. It builds slowly through identifiable stages, from situational anxiety to persistent worry to a chronic state where you can’t remember what calm feels like.
That gradual onset makes it easy to overlook until you’re completely exhausted.
Panic Disorder: When Your Body Convinces You You’re Dying
What a panic attack actually is (clinically)
A panic attack is a sudden surge of intense fear that peaks within minutes.
Your heart pounds. Your chest tightens. You can’t catch your breath. You’re dizzy, trembling, sweating. Your hands tingle. You’re convinced, absolutely certain, that you’re having a heart attack, losing control, or dying.
Then, usually within 10-15 minutes, it passes.
Here’s what makes panic attacks particularly cruel: They feel life-threatening but are medically safe. Your body is doing exactly what it would do if a lion appeared, mobilising every system for immediate survival. Except there’s no lion. Just your racing thoughts in the cereal aisle at Tesco.
Panic disorder vs. occasional panic symptoms
Here’s where we separate panic attacks from Panic Disorder:
Lots of people experience a panic attack at some point. One-off panic attacks are actually quite common, usually triggered by significant stress, lack of sleep, or too much caffeine.
Panic Disorder is diagnosed when:
- Panic attacks are recurrent and unexpected (you can’t predict when they’ll hit)
- You develop persistent fear of having another attack
- You change your behaviour to avoid perceived triggers
- This pattern continues for at least a month
The disorder isn’t maintained by external danger. It’s maintained by fear of the panic itself.
You become hypervigilant to your own body sensations. That flutter in your chest? Must be another panic attack starting. You avoid anywhere you’ve panicked before, that supermarket, that Tube line, that friend’s house.
Your world gradually shrinks.
Panic attacks vs. anxiety attacks (yes, they’re different)
People use these terms interchangeably. They shouldn’t.
Panic attacks are sudden and intense. They hit you like a freight train, zero to terror in seconds. They peak quickly, usually within 10 minutes.
Anxiety attacks build gradually. They’re linked to ongoing stress or worry. They feel more like a slow simmer that eventually boils over.
Why does this distinction matter? Treatment approaches differ. Panic disorder responds particularly well to interoceptive exposure (deliberately triggering the sensations you fear). General anxiety might need broader cognitive work.
Social Anxiety Disorder: More Than Just Shyness
Why social anxiety isn’t the same as being introverted
Let’s separate three things that constantly get confused:
Shyness is a personality trait. You’re quiet in new situations, prefer small groups, feel a bit awkward at parties. But you can do it. You don’t avoid social situations altogether.
Introversion is an energy preference. Social interaction drains you; you need alone time to recharge. Nothing to do with fear.
Social Anxiety Disorder is intense fear of being judged, embarrassed, or negatively evaluated in social situations.
Here’s the difference: Social anxiety is driven by fear, not preference.
In social anxiety:
- The fear is excessive and persistent you’re not just a bit nervous, you’re convinced everyone sees you as awkward, boring, or incompetent
- You actively avoid social situations or endure them with significant distress
- Your functioning at work, education, or relationships is impaired
- Physical symptoms kick in hard: blushing, sweating, trembling, nausea
You want social connection. But the fear of judgment is so overwhelming that isolation feels safer.
Overcoming social anxiety becomes much easier when you understand the process behind it, not just the symptoms. Our guide to overcoming social anxiety explains this process step by step, helping you make real, lasting progress.
Performance vs. generalised social anxiety
Social anxiety shows up in two main patterns:
Performance-based social anxiety affects specific situations such as public speaking, presentations, performing in front of others. You’re fine in casual conversation but terrified of formal evaluation.
Generalised social anxiety affects most social interactions. Small talk at the coffee machine feels as threatening as presenting to the board. Making a phone call requires two hours of mental preparation.
Both forms can significantly limit your opportunities and self-confidence. The person who turned down a promotion to avoid presentations? Performance social anxiety. The talented professional working below their capability because they can’t network? Likely generalised.
Neither is “just shyness.”
Specific Phobias: When Fear of One Thing Controls Your Life
What makes a fear a “phobia”
Everyone’s afraid of something. That’s not a phobia.
A specific phobia involves intense, immediate fear of particular objects or situations that’s wildly disproportionate to actual risk.
Common specific phobias:
- Flying (aviophobia)
- Heights (acrophobia)
- Injections or blood (trypanophobia, hemophobia)
- Animals, dogs, spiders, snakes
- Enclosed spaces (claustrophobia)
Here’s what distinguishes a phobia from reasonable caution: You know the fear is excessive. Your logical brain says “this lift is safe,” but your fear brain screams “GET OUT NOW.”
The fear is immediate and overwhelming. You don’t gradually get nervous; you see the spider and terror hits instantly.
Why avoidance makes phobias worse
Here’s the trap most people fall into:
Avoidance works brilliantly in the short term. You avoid flying, you don’t feel anxious. Problem solved, right?
Wrong!
Avoidance temporarily reduces anxiety but reinforces your brain’s belief that the feared object is actually dangerous. Every time you avoid, you’re teaching your brain: “See? We were right to be terrified. Good thing we didn’t go near that.”
Over time, avoidance doesn’t just maintain the phobia it strengthens it. The fear spreads to related situations. Started with a fear of large dogs? Now you’re crossing the street to avoid any dog. Won’t use lifts? Now you’re avoiding tall buildings entirely.
Phobias often remain stable across years unless actively treated. They don’t just “get better” with time. But here’s the good news: Specific phobias respond exceptionally well to targeted exposure therapy. Better success rates than almost any other anxiety disorder.
Agoraphobia: Not What You Think It Is
What agoraphobia actually involves
Most people think agoraphobia means “fear of open spaces” or “fear of leaving the house.”
Not quite.
Agoraphobia is fear of being in situations where escape might be difficult or help might not be available if panic symptoms occur.
Commonly avoided situations include:
- Public transport (buses, trains, Underground)
- Crowded places (shopping centres, queues, concerts)
- Open spaces (car parks, bridges, fields)
- Enclosed spaces (shops, cinemas, lifts)
- Being outside the home alone
Notice the pattern? It’s not about the space itself. It’s about feeling trapped or unable to get help if something goes wrong.
How agoraphobia and panic disorder feed each other
Here’s the typical progression:
You have a panic attack on the Tube. Terrifying experience. Next time you need the Tube, you feel anxious. Then you have another panic attack. Now your brain links “Tube” with “danger.”
So you avoid the Tube. Then you have a panic attack on a bus. Now buses are out. Then in a shop. Then walking to the shop.
Your world gradually shrinks until “safe” is just your home or even just your bedroom.
Not everyone with panic disorder develops agoraphobia. But when agoraphobia develops, it’s usually following repeated panic attacks in public places.
The combination is particularly debilitating. You’re not just afraid of panic attacks you’re afraid of having them in places where you feel exposed, trapped, or far from safety.
Separation Anxiety Disorder: Not Just for Children
How separation anxiety presents in kids
Separation Anxiety Disorder involves excessive fear related to separation from attachment figures usually parents or primary caregivers.
In children, this looks like:
- Extreme distress at school drop-off that goes beyond normal adjustment
- Persistent fear that something bad will happen to parents (accidents, illness, death)
- Physical symptoms when separated, stomach aches, headaches, nausea
- Nightmares about separation
- Refusal to sleep away from home or alone
Some separation anxiety is developmentally normal. Toddlers going through a clingy phase? Expected. The disorder is defined by severity and persistence, when it continues beyond the developmental stage and significantly impairs functioning.
Adult separation anxiety (yes, it’s real)
Here’s what most people don’t know: Separation anxiety can persist into adulthood or emerge for the first time in adults.
Adult separation anxiety affects:
- Romantic relationships (constant need for reassurance, difficulty with partner’s travel)
- Independence (extreme discomfort being home alone, difficulty making autonomous decisions)
- Occupational functioning (turning down opportunities that require travel or relocation)
Adult separation anxiety is often completely overlooked. Partners may be labelled “clingy” or “controlling” when they’re actually experiencing genuine anxiety disorder. The person knows their fear is excessive but can’t switch it off.
It’s highly impairing and entirely treatable, when properly identified.
Selective Mutism: When Anxiety Steals Your Voice
What selective mutism actually is
Selective mutism is an anxiety disorder where individuals are unable to speak in certain social settings despite having completely normal language ability.
This typically shows up in:
- School environments
- Public settings
- Interactions with unfamiliar people
The same child who won’t speak at school is chatting away at home. Speech is intact in safe environments; anxiety blocks it in others.
Why it’s not a communication disorder
Selective mutism is driven by anxiety, not by language deficits or cognitive impairment.
This distinction matters enormously. Without proper recognition, selective mutism may be mistaken for:
- Oppositional behaviour (“she’s just being stubborn”)
- Developmental delay
- Autism spectrum disorder (though they can co-exist)
- Hearing problems
Children with selective mutism aren’t choosing silence to be difficult. The anxiety is so overwhelming that speaking feels impossible, like trying to speak while someone’s choking you.
Early intervention is crucial. Left untreated, selective mutism can persist into adolescence and adulthood, significantly impairing social development and opportunities.
When Anxiety Disorders Overlap (Spoiler: Often)
Here’s the reality: Many people experience more than one type of anxiety disorder simultaneously.
Common combinations:
- GAD alongside social anxiety
- Panic disorder with agoraphobia (extremely common)
- GAD with panic disorder
- Specific phobias with GAD
Add to this: Anxiety disorders frequently co-exist with depression, trauma-related conditions (particularly PTSD), OCD, and eating disorders.
This isn’t diagnostic confusion or sloppy assessment. Overlap reflects shared underlying vulnerabilities, genetic factors, brain chemistry, learned patterns, early experiences.
Why this matters for treatment: You can’t just address one anxiety disorder and assume the others will resolve. Comprehensive assessment identifies all presenting conditions, allowing treatment to be properly targeted and sequenced.
Why Getting the Right Diagnosis Actually Changes Everything
Let’s be honest about what happens when anxiety is misidentified:
You try treatment that doesn’t quite fit. Maybe CBT that focuses on thought challenging when you actually need exposure work. Maybe medication that helps a bit but doesn’t touch your core symptoms.
You feel frustrated. You start wondering if you’re “treatment-resistant” or if anxiety “just can’t be treated” for you.
You lose confidence in mental health care. You’ve tried, it didn’t work, what’s the point?
Accurate identification matters because treatments vary significantly between disorders.
Social anxiety responds exceptionally well to specific CBT protocols that wouldn’t be appropriate for GAD. Panic disorder needs interoceptive exposure. Specific phobias need graded exposure to the feared object. GAD might need acceptance-based approaches alongside worry management.
Medication responses differ too. SSRIs work well across most anxiety disorders, but propranolol is particularly useful for performance anxiety. Benzodiazepines might be appropriate for occasional panic attacks but problematic for GAD.
Prognosis depends on early, accurate intervention. Anxiety disorders that are properly identified and treated early have excellent outcomes. Left to entrench, they become harder to treat and more likely to trigger secondary problems like depression or substance use.
You deserve treatment that actually fits what you’re experiencing.
What a Proper Anxiety Assessment Looks Like
What happens in a comprehensive psychiatric assessment for anxiety
A proper assessment isn’t a 15-minute GP appointment with a standardised questionnaire. It’s a detailed clinical evaluation that explores:
Symptom history and progression: When did this start? How has it changed? What makes it better or worse?
Triggers and maintaining factors: What situations trigger your anxiety? What keeps it going? What have you tried?
Functional impact: How is this affecting your work, relationships, daily life, physical health?
Personal and family mental health history: Have you experienced this before? Is there family history of anxiety or other mental health conditions?
Physical health and medications: Medical conditions that can mimic or worsen anxiety, medications that might contribute, substance use.
The assessment considers both type of anxiety disorder and stage is this situational and recent, or chronic and entrenched?
This takes time. Usually 60-90 minutes for initial assessment, sometimes longer for complex presentations.
Why self-diagnosis has real limitations
Look, self-education is valuable. Understanding anxiety disorders helps you advocate for yourself and make informed decisions.
But self-diagnosis can:
- Oversimplify complex presentations (you might identify one anxiety disorder but miss others)
- Miss co-existing conditions (particularly depression or trauma)
- Lead to inappropriate self-treatment
- Cause unnecessary worry about conditions you don’t have
Professional assessment provides clarity, formulation, and direction. It’s not about validation or labels, it’s about getting the right treatment approach from the start.
When to Actually Seek Professional Help
You should consider professional assessment if:
Anxiety persists for months despite your best efforts to manage it yourself
Avoidance is increasing, your world is gradually shrinking, you’re making decisions based on anxiety
Daily functioning is affected, work performance declining, relationships strained, activities abandoned
Physical symptoms are frequent, chest pain, breathlessness, GI issues (get medical clearance first)
Reassurance no longer helps, people tell you “it’ll be fine” and it makes zero difference
You’re using alcohol or other substances to cope
Early assessment prevents anxiety from becoming deeply entrenched. The earlier you intervene, the faster and more complete the recovery.
UK pathways to get help
Your options depend on severity, complexity, and urgency:
GP referral to NHS psychological services: Free, but waiting times currently 6-18 months in most areas. Suitable if anxiety is moderate and you can wait.
Self-referral to NHS IAPT services: Faster access, usually 4-8 weeks, but limited to low-moderate anxiety and specific conditions.
Private psychiatric assessment: £300-600 for initial assessment, immediate access, comprehensive evaluation including medication options if appropriate.
Private psychology/psychotherapy: Direct access to therapists, £80-150 per session, no waiting.
There’s no “right” pathway, it depends on what you need and what’s accessible to you. The important thing is starting somewhere rather than waiting for crisis point.
The Bottom Line: Clarity Makes Recovery Possible
Here’s what you need to remember:
Anxiety disorders are not a single condition. There are seven distinct types, each with unique features, mechanisms, and treatment needs.
Anxiety progresses through identifiable stages, from situational to persistent to entrenched. Catching it earlier makes treatment faster and more effective.
Accurate assessment improves outcomes. When treatment matches your specific condition, you get better results with less frustration.
Overlap is common. Multiple anxiety disorders can co-exist. That doesn’t mean you’re “worse” or “complicated”, it means thorough assessment is even more important.
Effective treatment exists. Anxiety disorders are among the most treatable mental health conditions. With proper identification and targeted intervention, most people experience significant improvement.
You don’t need to struggle with vague, generic “anxiety” forever. Clarity replaces confusion. Understanding replaces dismissal. Recovery becomes not just possible, but achievable. The first step is knowing exactly what you’re dealing with. Now you do.